My father was college-educated and had no obvious difficulty understanding medical advice in his earlier years. However, when he began to develop dementia there was a very noticeable change in his intellectual capacity. When I accompanied him to doctor visits, I noticed that not only did he struggle with understanding his instructions, he was also impaired in his ability to provide a detailed and accurate history to the physician. It was not uncommon for him to give one-word replies to questions that warranted detailed explanations. When I would “quiz” him after the visit about things the doctor said, he usually said he didn’t remember. These gaps could have led to devastating health consequences. Patients who don’t understand their medical instructions are at risk for medication errors, worsening of chronic conditions, and unnecessary hospitalizations. You may be surprised to learn that many without dementia or other chronic conditions are unable to effectively navigate the health care system due to what is known as low health literacy.
The National Library of Medicine defines health literacy as “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.” Health literacy goes far beyond one’s ability to read. It encompasses reading, writing, basic mathematical calculations, speaking, listening, networking, and the ability to comprehend rhetoric. The U.S. health care system is extremely complicated. As such, those who are well-educated struggle to understand insurance benefits and medication instructions. This problem is magnified for individuals with even minor intellectual disabilities.
According to the National Assessment of Adult Literacy, only 12 percent of Americans 16 years of age and older has proficient health literacy. Low health literacy is a problem that spans across all socioeconomic and racial groups. However, individuals with physical and mental disabilities, those who are non-white, the elderly, individuals with limited English proficiency, and those with lower socioeconomic status and education are most at risk.
Health literacy extends beyond traditional medical settings like your doctor’s office or the emergency room. We make health-related decisions on a daily basis, from reading nutrition labels in the grocery store to filtering information on the Internet. Health literacy extends across all domains of our daily lives.
It is important to understand that health literacy includes numeracy, the ability to understand and work with numbers. That’s right everyone, it involves doing MATH! I don’t have to tell you how many Americans struggle with math skills. It turns out these skills aren’t just important for engineers and statisticians. Individuals who are unable to perform basic multiplication and division calculations will have difficulty managing some aspects of their health.
As an example, below is a food label for a can of soup:
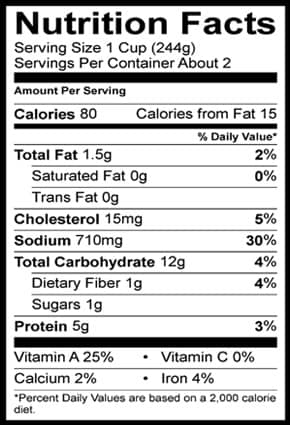
How many milligrams (mg) of sodium are in ½ cup of soup? If you were to eat the entire can of soup, how many calories would you consume?
(Answer: 355 mg, 160 calories)
Here’s another example of numeracy. Below is a medication label for Acetaminophen:
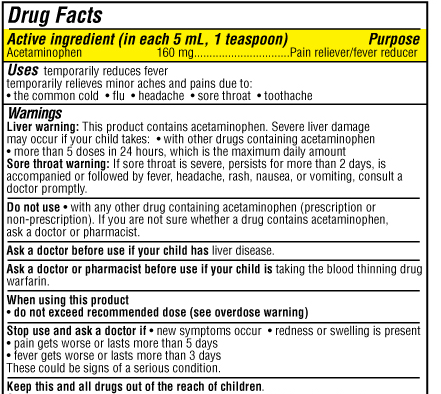
If your child’s pediatrician instructed you to give 320 mg of Acetaminophen, how many teaspoons would you give?
Answer: 2 teaspoons
These examples illustrate how individuals with limited math ability may experience significant difficulty making important decisions related to their health and that of their family members.
Unfortunately, despite the importance of health literacy, it is rarely discussed. Health care providers are under time constraints that make it difficult to reliably assess the health literacy of individual patients. Patients who have difficulty reading, understanding, or performing math operations often feel ashamed and embarrassed and are not likely to communicate this to their physicians. The onus is on those of us working in the health care field to ensure we are communicating clearly and that we assess our patient’s ability to understand and carry out our recommendations. But patients and caregivers, I’m not letting you completely off the hook. You also need to speak up- – be sure you understand what you are being told BEFORE you exit your medical encounters.
There are tools available to help patients with health literacy. I really like the Ask Me 3 campaign by the National Patient Safety Foundation (NPSF). It highlights three questions that patients and family members should ask their health care providers at every visit:
-
What is my main problem?
-
What do I need to do?
-
Why is it important for me to do this?

Image credit: NPSF (www.npsf.org)
To learn more, check out my 3-part series on the 3 Questions You Must Ask at Every Doctor’s Visit: Part 1, Part 2, and Part 3.
Do you understand what your doctor is saying to you? If you consistently ask these three questions, you will be well on your way to improving your ability to communicate with your health care providers, your knowledge of your medical conditions, and your health status.
Have you joined the Your GPS Doc Family? If not, please click here to receive notifications about new content as well as useful worksheets and additional resources only available to Your GPS Doc subscribers.






t thoughts. Thank you for sharing informative ideas regarding in this matter.
You’re very welcome! Thanks for reading.